Addressing inequalities within a rapidly ageing global population
Addressing inequalities within a rapidly ageing global population
To address a rapidly ageing global population, governments, civil society and individuals have had to come together to work towards creating a world of healthy older people whose rights and choices are both protected and respected.
Organizations committed to advancing the rights of older people around the world have made tremendous strides, as demonstrated by the breadth and quality of work presented at the IFA 14th Global Conference on Ageing. Advancements toward promoting healthy ageing, developing and maintaining age-friendly cities and communities, and new initiatives to combat ageism have all emerged in recent years and continue to improve the health and wellbeing of older people globally.
Yet, global inequalities persist that threaten these improvements. Society often understates the fact that life experiences significantly impact, and at times jeopardize, the health and ability of older people to meet their basic needs. Also, certain subpopulations of older people experience additional marginalization, which is known to further impact their lives.
 In August 2018, the IFA in collaboration with the Government of Canada, hosted a pre-conference Addressing Inequalities Summit that fostered discussions among participants interested in and committed to eliminating inequalities experienced by older people within marginalized subpopulations. The summit explored the experiences of older women, older Indigenous people, older prisoners, older immigrants, older people living in rural and remote areas, older homeless people and older LGBTQ2 people.
In August 2018, the IFA in collaboration with the Government of Canada, hosted a pre-conference Addressing Inequalities Summit that fostered discussions among participants interested in and committed to eliminating inequalities experienced by older people within marginalized subpopulations. The summit explored the experiences of older women, older Indigenous people, older prisoners, older immigrants, older people living in rural and remote areas, older homeless people and older LGBTQ2 people.
Building on the new learnings gained during the event, a post-summit report was created that highlights the experiences of identified groups of older people, successful best practices and next steps for addressing inequalities experienced by marginalized subpopulations of older people. The full report can be accessed here.
The themes and next steps identified within the Addressing Inequalities Summit report have the potential to be applied to all research impacting older people. As the IFA and other organizations move into 2019, working towards promoting the rights of older people globally, it is critical that a conscious effort is made to ensure the diverse experiences of marginalized older people are included in policy and practice.


Care, an age-old problem
What goes without saying is that older people have a depleting health that needs constant care and management. The problems could range from debilitating joint pain and constant coughing to life-threatening heart diseases and cancer. A 2011 report by the Ministry of Social Justice shows that 160 of every 1,000 elderly living in urban areas suffer from heart diseases. Urinary problems are more common among aged men, while most aged women suffer from joint problems. Of every 1,000 elderly, nearly 64 in rural and 55 in urban areas have one or the other form of disability, such as hearing difficulty, poor vision or locomotive impairment.
Lately, depression has emerged as another common ailment among the aged. According to a study published in Neurosciences in Rural Practice in 2011, about 22 per cent of the elderly in India—or every fifth elderly in the country—are depressed. The worldwide average is 10.3 per cent. The study, led by Ankur Barua of Melaka-Manipal Medical College, Malaysia, analysed figures from Asia, Europe, Australia, North America and South America. This is a scary situation because more often than not an elderly suffers from more than one disease.

“These are the problems of old-age and are interrelated. There is natural decay of the body and every ailment need not be treated the way it is done for other age groups,” says A B Dey, head of the geriatrics department at AIIMS. “So, there is a need for geriatricians who are trained to see the person in the context of age and give less medicine for maximum advantage.” Besides, Dey says, most elderly are not aware of their illnesses, even if they are at a later stage of life-threatening diseases like heart problems and cancer. They think the symptoms are part of the ageing process. Between July 2012 and July 2013, his department and the Indian Council of Medical Research assessed the health of 1,643 above-60 people who visited the general out-patient department of AIIMS and followed them up for one year. To their surprise, they found only 15 per cent patients alive by the end of the year; 30 per cent died within the first month of treatment. “We now check patients for a set of diseases even if they approach us for some other ailment,” he adds.
 For someone like Urmila Devi, who suffers from high blood pressure, diabetes and neurological disorder, visiting a geriatrician would not only save her from the trouble of approaching multiple doctors and save precious pension money, she would also be diagnosed of any hidden disease before it is too late. But a geriatrician is not easy to come by.
For someone like Urmila Devi, who suffers from high blood pressure, diabetes and neurological disorder, visiting a geriatrician would not only save her from the trouble of approaching multiple doctors and save precious pension money, she would also be diagnosed of any hidden disease before it is too late. But a geriatrician is not easy to come by.
Heartless attempt
Much hope was pinned on the Union health ministry when it opened National Programme for Health Care of the Elderly (NPHCE) in June 2010. It is the first programme with special focus on the health requirement of the aged. Under NPHCE, the ministry promised to establish geriatric departments in eight super-specialised hospitals and strengthening healthcare facilities for the elderly in each district. Under the first phase (2010-2012), NPHCE was planned to cover 100 districts of 21 states and union territories. The remaining 540 districts were to be covered during 2012-17. But it is yet to keep its word.
Lov Verma, secretary of the ministry, told Down To Earth, “We have opened geriatric out-patient departments in eight hospitals and indoor (hospitalisation) services in six. We plan to open National Institutes of Ageing (nodal agency for research and healthcare) at AIIMS and Madras Medical College in Chennai.”
Doctors at the geriatric departments say they are yet to receive the promised Rs 20 lakh per annum, meant for subsidising medicines and tests. District-level implementation of the programme also remains a far cry.
The government’s apathy towards the elderly becomes evident from the fact that in 2012-13, the ministry released only Rs 1.15 crore of the Rs 50 crore allocated for the elderly under National Health Mission. The same year, the ministry released Rs 68.56 crore out of the allocated Rs 150 crore for NPHCE. However, the utilisation of the fund remains poor. According to a January 2014 report by industry body ASSOCHAM and KPMG, a company that offers advisory services, Kerala, the state with one of the largest elderly populations, has utilised only 8 per cent of the Rs 8.79 crore received under NPHCE.
Such apathy comes as no surprise in a country that drafted its National Policy on Older Persons only in 1999. “The policy, meant to address issues relating to ageing in a comprehensive manner, failed to provide relief to the elderly, primarily due to lack of focus of the government and no will towards its implementation,” says Cherian.
Financial crunch, health problems and living alone have emerged as the top three fears of the elderly, according to the ASSOCHAM-KPMG report. And cashing in on these are the real estate sector and private healthcare facilities.
With attitude towards the elderly changing, the business of care booms

Elderly & lonely
India has more elderly people than ever before. Most of them have little social security and cannot afford healthcare. While the government seems ill-prepared to provide them care, private players are rushing to offer expensive facilities and services. Jyotsna Singh reports
By Jyotsna Singh
Last Updated: Thursday 01 October 2015
Elderly & lonely

Living to a ripe old age should be a cause for celebration. Alas, it was not so for Usha John, once a sprightly, hard-working and fiercely independent IAS officer. After retirement, John lived in her bungalow in the upmarket Hauz Khas of Delhi, aided by a few housekeepers. But over the years, they deserted her. “In March, I received a call from one of her neighbours who informed that they had not seen any activity in John’s house for a long time,” says Mathew Cherian, chief executive of HelpAge India, a non-profit working for the rights of the elderly. “When we visited her house, we discovered a frail figure.” She was barely 19 kg. Cherian rushed her to the All India Institute of Medical Sciences (AIIMS), where the doctors informed that she had hardly eaten anything for two to three months and was suffering from cancer. The 85-year-old spinster died in the hospital a month later. Some relatives of her sister, who lives in Mumbai, came to complete hospital formalities.
Unlike John, 82-year-old Urmila Devi has two sons who are doing quite well for themselves. Yet she is living out her dotage in an old-age home in Kanjhawala in north-west Delhi. Her sons live in the same city, but no one has come looking for her in the past three years, say attendants at the old-age home, run by Triveni Devi Charitable Society. “Since the death of my husband 10 years ago, I have developed some mental disorder and tend to forget eating or taking medicines on time,” says Devi, flipping through the photographs from her younger days, kept carefully by bedside. “My children would often speak harsh words for being a burden on the family.” She left home after one such tiff with her son’s family.
 There is no dearth of such stories of loss and loneliness in the country, which is undergoing a rapid transformation—both socially and demographically.
There is no dearth of such stories of loss and loneliness in the country, which is undergoing a rapid transformation—both socially and demographically.
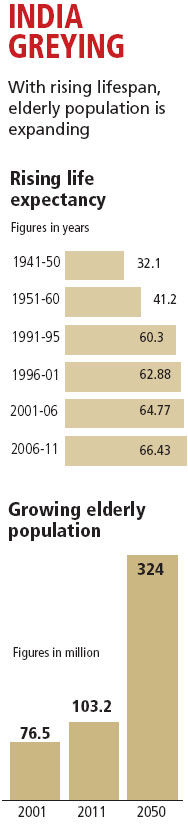
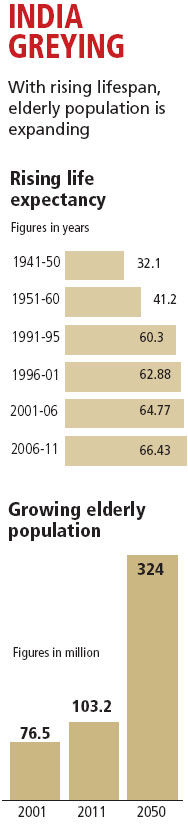
Due to improved healthcare worldwide, the average lifespan of an individual has increased in the last few decades. India is no exception. According to the Census of India, the life expectancy of an Indian was 52 in 1975. Today, an average Indian man lives beyond 67 years and women about 70 years, according to the Union Ministry of Health and Family Welfare. There is, however, a downside to the success story. Increased longevity means there are more elderly people than before. From 56.5 million in 1991, the number of elderly (those above 60) has increased to 103.2 million in 2011—the largest ever in the country’s history. According to the Union Ministry of Statistics and Programme Implementation (MoSPI), by 2050 a greying India will have a quarter of its population to look after. A sizeable portion of them would be very old (80 and above) and widows, as women tend to live longer. Most of this ailing, frail population would be living in villages (see ‘India greying’ and ‘State of our elders’).
Many other countries are witnessing similar demographic change. But the rapidly ageing population is a matter of worry for India because of two reasons. One, attitude towards the elderly is changing. Though India’s traditional piety requires children to look after their parents, nuclear families have little time or resources for their ailing parents. Increased migration from rural areas also forces the younger generation to leave their elders alone back home. Finances are stretched and healthcare expensive. Worse, nearly 90 per cent of the elderly worked in the informal sector and do not receive social security coverage, like pension and mediclaim, post retirement, according to HelpAge India. They either continue to work beyond retirement age or suffer from neglect and alienation.
Two, the government seems little bothered about the growing acuteness of the problem and ill-prepared for the mounting responsibility. Apathy of the political class is evident from the fact that the ruling United Progressive Alliance spent just 151 words for the elderly in its 81-page Report to the People 2012-13. There was no mention of the performance of the programmes for the elderly in the report. This is surprising because the average age of the Cabinet is 65 years. Even in this general election, the manifestos of major political parties pay mere lip service to the issues of the elderly.
Unlike John, 82-year-old Urmila Devi has two sons who are doing quite well for themselves. Yet she is living out her dotage in an old-age home in Kanjhawala in north-west Delhi. Her sons live in the same city, but no one has come looking for her in the past three years, say attendants at the old-age home, run by Triveni Devi Charitable Society. “Since the death of my husband 10 years ago, I have developed some mental disorder and tend to forget eating or taking medicines on time,” says Devi, flipping through the photographs from her younger days, kept carefully by bedside. “My children would often speak harsh words for being a burden on the family.” She left home after one such tiff with her son’s family.
 There is no dearth of such stories of loss and loneliness in the country, which is undergoing a rapid transformation—both socially and demographically.
There is no dearth of such stories of loss and loneliness in the country, which is undergoing a rapid transformation—both socially and demographically. Due to improved healthcare worldwide, the average lifespan of an individual has increased in the last few decades. India is no exception. According to the Census of India, the life expectancy of an Indian was 52 in 1975. Today, an average Indian man lives beyond 67 years and women about 70 years, according to the Union Ministry of Health and Family Welfare. There is, however, a downside to the success story. Increased longevity means there are more elderly people than before. From 56.5 million in 1991, the number of elderly (those above 60) has increased to 103.2 million in 2011—the largest ever in the country’s history. According to the Union Ministry of Statistics and Programme Implementation (MoSPI), by 2050 a greying India will have a quarter of its population to look after. A sizeable portion of them would be very old (80 and above) and widows, as women tend to live longer. Most of this ailing, frail population would be living in villages (see ‘India greying’ and ‘State of our elders’).
Many other countries are witnessing similar demographic change. But the rapidly ageing population is a matter of worry for India because of two reasons. One, attitude towards the elderly is changing. Though India’s traditional piety requires children to look after their parents, nuclear families have little time or resources for their ailing parents. Increased migration from rural areas also forces the younger generation to leave their elders alone back home. Finances are stretched and healthcare expensive. Worse, nearly 90 per cent of the elderly worked in the informal sector and do not receive social security coverage, like pension and mediclaim, post retirement, according to HelpAge India. They either continue to work beyond retirement age or suffer from neglect and alienation.
Two, the government seems little bothered about the growing acuteness of the problem and ill-prepared for the mounting responsibility. Apathy of the political class is evident from the fact that the ruling United Progressive Alliance spent just 151 words for the elderly in its 81-page Report to the People 2012-13. There was no mention of the performance of the programmes for the elderly in the report. This is surprising because the average age of the Cabinet is 65 years. Even in this general election, the manifestos of major political parties pay mere lip service to the issues of the elderly.

Care, an age-old problem
What goes without saying is that older people have a depleting health that needs constant care and management. The problems could range from debilitating joint pain and constant coughing to life-threatening heart diseases and cancer. A 2011 report by the Ministry of Social Justice shows that 160 of every 1,000 elderly living in urban areas suffer from heart diseases. Urinary problems are more common among aged men, while most aged women suffer from joint problems. Of every 1,000 elderly, nearly 64 in rural and 55 in urban areas have one or the other form of disability, such as hearing difficulty, poor vision or locomotive impairment.
Lately, depression has emerged as another common ailment among the aged. According to a study published in Neurosciences in Rural Practice in 2011, about 22 per cent of the elderly in India—or every fifth elderly in the country—are depressed. The worldwide average is 10.3 per cent. The study, led by Ankur Barua of Melaka-Manipal Medical College, Malaysia, analysed figures from Asia, Europe, Australia, North America and South America. This is a scary situation because more often than not an elderly suffers from more than one disease.

“These are the problems of old-age and are interrelated. There is natural decay of the body and every ailment need not be treated the way it is done for other age groups,” says A B Dey, head of the geriatrics department at AIIMS. “So, there is a need for geriatricians who are trained to see the person in the context of age and give less medicine for maximum advantage.” Besides, Dey says, most elderly are not aware of their illnesses, even if they are at a later stage of life-threatening diseases like heart problems and cancer. They think the symptoms are part of the ageing process. Between July 2012 and July 2013, his department and the Indian Council of Medical Research assessed the health of 1,643 above-60 people who visited the general out-patient department of AIIMS and followed them up for one year. To their surprise, they found only 15 per cent patients alive by the end of the year; 30 per cent died within the first month of treatment. “We now check patients for a set of diseases even if they approach us for some other ailment,” he adds.
 For someone like Urmila Devi, who suffers from high blood pressure, diabetes and neurological disorder, visiting a geriatrician would not only save her from the trouble of approaching multiple doctors and save precious pension money, she would also be diagnosed of any hidden disease before it is too late. But a geriatrician is not easy to come by.
For someone like Urmila Devi, who suffers from high blood pressure, diabetes and neurological disorder, visiting a geriatrician would not only save her from the trouble of approaching multiple doctors and save precious pension money, she would also be diagnosed of any hidden disease before it is too late. But a geriatrician is not easy to come by. Heartless attempt
Much hope was pinned on the Union health ministry when it opened National Programme for Health Care of the Elderly (NPHCE) in June 2010. It is the first programme with special focus on the health requirement of the aged. Under NPHCE, the ministry promised to establish geriatric departments in eight super-specialised hospitals and strengthening healthcare facilities for the elderly in each district. Under the first phase (2010-2012), NPHCE was planned to cover 100 districts of 21 states and union territories. The remaining 540 districts were to be covered during 2012-17. But it is yet to keep its word.
Lov Verma, secretary of the ministry, told Down To Earth, “We have opened geriatric out-patient departments in eight hospitals and indoor (hospitalisation) services in six. We plan to open National Institutes of Ageing (nodal agency for research and healthcare) at AIIMS and Madras Medical College in Chennai.”
Doctors at the geriatric departments say they are yet to receive the promised Rs 20 lakh per annum, meant for subsidising medicines and tests. District-level implementation of the programme also remains a far cry.
The government’s apathy towards the elderly becomes evident from the fact that in 2012-13, the ministry released only Rs 1.15 crore of the Rs 50 crore allocated for the elderly under National Health Mission. The same year, the ministry released Rs 68.56 crore out of the allocated Rs 150 crore for NPHCE. However, the utilisation of the fund remains poor. According to a January 2014 report by industry body ASSOCHAM and KPMG, a company that offers advisory services, Kerala, the state with one of the largest elderly populations, has utilised only 8 per cent of the Rs 8.79 crore received under NPHCE.
Such apathy comes as no surprise in a country that drafted its National Policy on Older Persons only in 1999. “The policy, meant to address issues relating to ageing in a comprehensive manner, failed to provide relief to the elderly, primarily due to lack of focus of the government and no will towards its implementation,” says Cherian.
Financial crunch, health problems and living alone have emerged as the top three fears of the elderly, according to the ASSOCHAM-KPMG report. And cashing in on these are the real estate sector and private healthcare facilities.
Home, old-age home
With attitude towards the elderly changing, the business of care booms

Vandana Das (name changed), 71, did not realise when her behaviour changed. She became rude and withdrawn, and could not manage her daily chores. Doctors diagnosed her of suffering from dementia. The son, a bank executive in Pune, bought a two-bedroom flat in a retirement colony and moved his mother there. She is now under the full-time care of a nurse.
The widening gap between the elderly and their children has opened new avenues for private players who have introduced concepts of elderly care at home to retirement homes.
People in their late 30s and 40s are encouraged to invest in retirement homes. According to a 2011 report by Jones Lang LaSalle India, a real estate consulting company, the current demand for retirement homes is 300,000 units. “Indian market has only 4,000-5,000 such units, catering to less than 2 per cent of the demand,” says Ankur Gupta. He is joint managing director of one such housing colony, Ashiana Utsav in Bhiwadi township in Rajasthan’s Alwar district.
A gated community with double security check for every visitor, Ashiana Utsav provides architecture, facilities and services for people above 55. It has 650 flats, of which 458 are occupied by old couples and singles. Corridors are equipped with soft-textured handrails to provide extra support to the very old people. Special care is being taken to ensure that electricity is available round-the-clock and lifts are always functional. “If you have not seen old age you really do not know what relaxation feels like,” reads a wall-hanging in the activity centre.
The widening gap between the elderly and their children has opened new avenues for private players who have introduced concepts of elderly care at home to retirement homes.
People in their late 30s and 40s are encouraged to invest in retirement homes. According to a 2011 report by Jones Lang LaSalle India, a real estate consulting company, the current demand for retirement homes is 300,000 units. “Indian market has only 4,000-5,000 such units, catering to less than 2 per cent of the demand,” says Ankur Gupta. He is joint managing director of one such housing colony, Ashiana Utsav in Bhiwadi township in Rajasthan’s Alwar district.
A gated community with double security check for every visitor, Ashiana Utsav provides architecture, facilities and services for people above 55. It has 650 flats, of which 458 are occupied by old couples and singles. Corridors are equipped with soft-textured handrails to provide extra support to the very old people. Special care is being taken to ensure that electricity is available round-the-clock and lifts are always functional. “If you have not seen old age you really do not know what relaxation feels like,” reads a wall-hanging in the activity centre.
This was precisely what was in the mind of Subhash Chandra Tyagi while he was looking for a house to settle down after retiring from a government eye hospital in Modinagar, Uttar Pradesh, as medical superintendent. “Our balcony opens to the park where we spend hours sipping tea, reading and talking to all the passers-by,” says Subhash. “Companionship is the primary need in old age,” says Suman, his wife. “Understanding this aspect, the colony developers have connected all flats with free intercom.”


The staff of 10 organises different activities for the residents, rekindling their long-dead hobbies and interests. Subhash has taken to playing guitar, a hobby that had once made him apple of everyone’s eye in his medical college. “We also organise cultural and religious activities, talks on health-related topics, outings and a monthly get-together to celebrate all birthdays and marriage anniversaries of that month,” says Devdeep, activities manager.
Tyagi bought the three-bedroom flat for Rs 12 lakh in 2004. Today, its cost is Rs 30 lakh. In addition, he pays Rs 2,500 as maintenance charge every month. This is an expensive proposition for most elderly people, who are poor or belong to lower-middle class section. For them, there are just 700-odd old-age homes across the country. According to Delhi non-profit Dada-Dadi, 325 of them are managed by charitable societies with the help of government and provide free-of-cost stay facilities. The rest are managed by private players. But getting a bed in an old-age home is as arduous an exercise as surviving the old age.
“Old-age homes and retirement homes should be treated as shelters, not long-term care homes,” says Dey. “Such arrangements are good for people till they are 75 years old. After that they need continued care and management.” Neither retirement homes nor old-age homes have such arrangements and the residents are visited by a general physician once or twice a week. The closest tertiary hospital to Ashiana Utsav is in Manesar, a 40-minute drive from Bhiwadi.
Home care solutions
Home care solutions are also emerging as a response to the need of the elderly. Epoch Elder Care is one such company in Gurgaon, Haryana. “Our Elder Care Specialists (ECS) offer intellectual companionship to the elderly at their homes,” says Tanvi Dalal, head of human resources at Epoch Elder Care. They accompany the elderly on outings, read and discuss articles with them, play games, help them go back to their hobbies and discover new ones, assist with email, Facebook and Skype, help them blog about their topics of interest and share stories. We also provide them health management and check-ups for blood pressure and blood sugar. For patients of dementia and Alzheimer’s, full-time trained attendants are available,” says Dalal. There is a high demand for attendants for the elderly and it is a great career potential, she adds. Depending on the length and number of sessions and services, hiring an ECS can cost between Rs 12,000 and Rs 14,000 a month.

Tyagi bought the three-bedroom flat for Rs 12 lakh in 2004. Today, its cost is Rs 30 lakh. In addition, he pays Rs 2,500 as maintenance charge every month. This is an expensive proposition for most elderly people, who are poor or belong to lower-middle class section. For them, there are just 700-odd old-age homes across the country. According to Delhi non-profit Dada-Dadi, 325 of them are managed by charitable societies with the help of government and provide free-of-cost stay facilities. The rest are managed by private players. But getting a bed in an old-age home is as arduous an exercise as surviving the old age.
“Old-age homes and retirement homes should be treated as shelters, not long-term care homes,” says Dey. “Such arrangements are good for people till they are 75 years old. After that they need continued care and management.” Neither retirement homes nor old-age homes have such arrangements and the residents are visited by a general physician once or twice a week. The closest tertiary hospital to Ashiana Utsav is in Manesar, a 40-minute drive from Bhiwadi.
Home care solutions
Home care solutions are also emerging as a response to the need of the elderly. Epoch Elder Care is one such company in Gurgaon, Haryana. “Our Elder Care Specialists (ECS) offer intellectual companionship to the elderly at their homes,” says Tanvi Dalal, head of human resources at Epoch Elder Care. They accompany the elderly on outings, read and discuss articles with them, play games, help them go back to their hobbies and discover new ones, assist with email, Facebook and Skype, help them blog about their topics of interest and share stories. We also provide them health management and check-ups for blood pressure and blood sugar. For patients of dementia and Alzheimer’s, full-time trained attendants are available,” says Dalal. There is a high demand for attendants for the elderly and it is a great career potential, she adds. Depending on the length and number of sessions and services, hiring an ECS can cost between Rs 12,000 and Rs 14,000 a month.

A similar model, but relatively low-cost, is being tried by a Bhubaneshwar-based non-profit, Sushruta. It provides nurses at just Rs 5,000 a month. “Most of our nurses are women and from rural Odisha. We train them in elderly care,” says Rashmi Pandian, head of Sushruta. “Their stay and food is managed by the family they serve. We ensure that they get proper bed and clean bathroom and toilet, and are treated with dignity.”
But there is no conclusive evidence to prove that home-based care helps increase the lifespan of an elderly, according to a study published in Plos One in March 2014. Researchers from University College London (UCL) and the University of Oxford said this after reviewing 64 studies done in the past 20 years on elders who received home care visits. Perhaps, nothing can replace the want to be with one’s own family.
Making use of the wisdom
To reduce generation gap between children, youth and the elderly, Ayaad Foundation, a not-for-profit company, has launched an innovative model in Kumbhalgarh in Rajasthan. It is building a residential complex in the tourist town. The elderly can book a residence for themselves. But unlike retirement homes, they will not own the property. They can stay there as long as they live, with the foundation taking care of their food and other day-to-day needs.
“There are two designs. One-bedroom cottages that can accommodate two-three people comes for Rs 12 lakh. Single rooms, meant for two persons, costs Rs 8 lakh,” says Nidhi Agarwal, founding member of Ayaad. The foundation plans to set up a facility for children with special abilities in the complex so that the elderly residents can keep themselves engaged by looking after them. “We also plan to bring children of migrant labourers and unemployed youth to the campus. The residents can assist them with education, work and skills. This way they use their knowledge and time and help society grow,” says Agarwal. The project is expected to be started by the end of the year.
How effective are models of care?
There is a growing interest for such models among a certain section of society. But analysts warn against them. “Till date there is no model catering to the complete range of old age needs like healthcare and productive ageing,” says Cherian. “The concept of retirement community is driven primarily by real estate developers, who lack skills and credibility in integrated living and lack understanding of age-specific care needs.”
But in the absence of a system to meet healthcare needs, like subsidised medicines, the elderly have nowhere to turn to (see box). In many cases, the meagre old-age pension received by a BPL elderly as a social welfare measure goes into buying medicines. Consider this. Every month Roshan Sahni, 78, a resident of Kalkaji area in Delhi, anxiously waits for per pension of Rs 1,000, which he receives under Indira Gandhi National Old Age Pension Scheme. “I am on medication for diabetes and hypertension for seven years. Last year, I was diagnosed with first stage lung cancer. I have been put on medicines for that too.” Sahni is lucky to be living with his son.
In the absence of a functioning national programme, a couple of municipal corporations have tried to intervene at their levels to provide healthcare to senior citizens. In 2003, Indore Municipal Corporation and in 2007, Gwalior Municipal Corporation initiated health insurance schemes for the elderly from poor financial backgrounds. It provided insurance cover of up to Rs 20,000 for hospitalisation expenses. But care for critical illnesses and medicines, that form a bulk of the medical expenses, are not part of the scheme. The ASSOCHAM-KPMG report says the scheme did not take off.
But there is no conclusive evidence to prove that home-based care helps increase the lifespan of an elderly, according to a study published in Plos One in March 2014. Researchers from University College London (UCL) and the University of Oxford said this after reviewing 64 studies done in the past 20 years on elders who received home care visits. Perhaps, nothing can replace the want to be with one’s own family.
Making use of the wisdom
To reduce generation gap between children, youth and the elderly, Ayaad Foundation, a not-for-profit company, has launched an innovative model in Kumbhalgarh in Rajasthan. It is building a residential complex in the tourist town. The elderly can book a residence for themselves. But unlike retirement homes, they will not own the property. They can stay there as long as they live, with the foundation taking care of their food and other day-to-day needs.
“There are two designs. One-bedroom cottages that can accommodate two-three people comes for Rs 12 lakh. Single rooms, meant for two persons, costs Rs 8 lakh,” says Nidhi Agarwal, founding member of Ayaad. The foundation plans to set up a facility for children with special abilities in the complex so that the elderly residents can keep themselves engaged by looking after them. “We also plan to bring children of migrant labourers and unemployed youth to the campus. The residents can assist them with education, work and skills. This way they use their knowledge and time and help society grow,” says Agarwal. The project is expected to be started by the end of the year.
How effective are models of care?
There is a growing interest for such models among a certain section of society. But analysts warn against them. “Till date there is no model catering to the complete range of old age needs like healthcare and productive ageing,” says Cherian. “The concept of retirement community is driven primarily by real estate developers, who lack skills and credibility in integrated living and lack understanding of age-specific care needs.”
But in the absence of a system to meet healthcare needs, like subsidised medicines, the elderly have nowhere to turn to (see box). In many cases, the meagre old-age pension received by a BPL elderly as a social welfare measure goes into buying medicines. Consider this. Every month Roshan Sahni, 78, a resident of Kalkaji area in Delhi, anxiously waits for per pension of Rs 1,000, which he receives under Indira Gandhi National Old Age Pension Scheme. “I am on medication for diabetes and hypertension for seven years. Last year, I was diagnosed with first stage lung cancer. I have been put on medicines for that too.” Sahni is lucky to be living with his son.
In the absence of a functioning national programme, a couple of municipal corporations have tried to intervene at their levels to provide healthcare to senior citizens. In 2003, Indore Municipal Corporation and in 2007, Gwalior Municipal Corporation initiated health insurance schemes for the elderly from poor financial backgrounds. It provided insurance cover of up to Rs 20,000 for hospitalisation expenses. But care for critical illnesses and medicines, that form a bulk of the medical expenses, are not part of the scheme. The ASSOCHAM-KPMG report says the scheme did not take off.


Comments